This post may contain affiliate links. Please read the disclosure.
As diabetic patients, it is often said that having A1C on our target is an important goal in diabetes management. But do you know why?
Do you know what the A1C’s target is, how to lower the A1C if necessary, how quickly you can safely lower the A1C?
What is A1c?
Also known as hemoglobin A1C, HBA1C, glycation hemoglobin, or glycohemoglobin, A1C is a blood test that measures the average blood glucose level over the past two to three months.
It’s not “average,” but rather a weighted average, with blood glucose levels over the past few weeks counting a little more than the blood glucose levels from two to three months ago.
According to the National Institute of Diabetes, Digestive and Kidney Disease (NIDDK):
It is important to note here that the term “normal A1C level” in this context refers to people without diabetes. I’m going back to what “normal A1C levels” are for people living with lower diabetes.
How to Test A1c
A physician or endocrinologist should check A1Cs regularly (usually every 3-6 months). The doctor simply stabs your finger and takes a small blood sample.
If you have an A1C kit in your doctor’s office, you should get results before the consultation is finished. (However, some offices send blood samples from the lab for processing.)
You can also purchase a Home A1C kit (no prescription required) and test it yourself. The Home A1C kit is useful if you want to monitor how A1C is trending if you go for more than three months between doctor visits.
Home kits are usually accurate within plus/minus 0.5 percent points. This is more than enough to provide reliable results.
The drawback of the Home Kit is that it requires more blood (typically a few large drops) than a regular blood glucose check, and if you don’t apply enough blood you will receive an error message and you will lose the A1C test strip.
You can find home test kits on Amazon and at select pharmacies. Make sure your home A1C kit is in use before its expiration date.
read more: How to measure A1C at home.
Why should you care about your A1c?
Several important studies have shown that high mean blood sugar increases the risk of diabetes-related complications. Reducing A1C to the recommended range reduces the risk of diabetes-related complications.
According to a follow-up study called Landmark Diabetes Control and Complications Trial (DCCT) and Diabetic Interventions and Complications Epidemiology (EDIC), diabetic patients who used in intensive care to keep A1C at target levels:
- The risk of eye disease has been reduced by 76%
- The risk of kidney disease has been reduced by 50%
- The risk of neurological diseases has been reduced by 60%
- The risk of cardiovascular events reduced by 42%
- The risk of non-fatal heart attacks, strokes, or death due to cardiovascular causes reduced by 57%
Therefore, achieving A1C within the recommended range is one of the most important things you can do to improve your long-term health when living with diabetes.
In some cases, lowering A1C may not be a good idea if it means increasing the frequency of experiencing hypoglycemia (hypoglycemia).
Later in this guide we will explain why the scale known as “in-range” (TIR) is just as important as a low-level A1C.
How to lower A1c
With a complete understanding of A1c, the obvious question is why it’s not best to see A1c alone.
How do you lower A1C while improving or maintaining time within range?
In my experience, I will explain the four most important things you can do below, but I recommend starting by talking to your healthcare team before making any changes to diabetes management.
Identify the main “problems”
Whether you are primarily self-managed with diabetes or working closely with your healthcare team, the first step is to always try to identify the main “problems” or identify reasons that are higher than A1C wants. The only real way to do this is to track your blood sugar levels very closely.
Wearing a continuous glucose monitor (CGM) allows you to look at blood glucose data for 7, 30, and 90 days to see if you can find trends.
For example, you can see that you run every morning from 1am to 5am, every morning (dawn phenomenon, early increase in glucose levels, etc.), or every day after meals. Or perhaps you will always be lower after exercise. We all have different blood sugar patterns.
It is also very likely that you will benefit from adjusting your diabetes medication just by constantly having a slightly higher blood sugar level.
Identifying such patterns allows for planning ways to limit hyperglycemia and hypoglycemia to identify areas of potential improvement.
If you rely on manual blood glucose monitoring, it’s a bit difficult, as most people don’t monitor it every 5 minutes. In this case, you can also check more frequently for a while, and check in the middle of the night if you wake up anyway.
Most meters allow you to download data to your computer or upload this data to one of a variety of app-based platforms. This will help you see your data in a more cohesive way, so you can start looking for trends.
Create a plan for diabetes management
Now that you have a better idea about what your “problems” are, you can start making changes to your diabetes management.
Your doctor may suggest another medication regime. For example, some people are prescribed metformin to aid in the dawn phenomenon. Others may need to be given insulin or other medication adjustments.
If you are using insulin and have consistently used hyperglycemia in the morning, if you have lowered blood glucose levels and A1c, it may be as easy as adjusting your nighttime basal (background) insulin.
Alternatively, running high every day after meals could turn off the insulin-carb ratio, and adjusting it could set you a path to a lower A1C. There is no way to know this until you collect data and do your analysis.
I would like to create an important point here. Increased diabetic medication is not a sign of failure. Often it is the best (sometimes only) way to manage your blood sugar levels and defeat A1c.
When changing your diet or exercise routine, always adjust your insulin up and down. The ability to regulate medication is an important tool in the diabetes toolbox and should always be discussed with your healthcare team.
Understand nutrition and regulate your diet
What you choose to eat or drink can have a major impact on your waistline, mood, happiness, and your blood sugar levels.
All macronutrients (carbohydrates, proteins, fats) can have some effect on your blood sugar levels, so having a good understanding of how they affect your blood sugar can help you become more active and prevent blood sugar shaking.
Carbohydrates (carbohydrates)
Carbohydrates have the most impact on blood sugar levels. Therefore, many people with diabetes can benefit from adopting a low-carb diet. The lower the carbohydrates you eat, the less insulin you need to take and easier diabetes management.
However, if it doesn’t work physically or mentally, you don’t need to follow a low-carb diet.
As I wrote in my work on which diet is best for people with diabetes, it is very possible to have excellent glucose control on a medium (or high) carbohydrate diet, as long as you learn to experiment, take notes, and take the right amount of insulin for the carbohydrates you are eating.
It is very important to recognize that we all respond differently to carbohydrates. That’s why you need to find the right food and food for you.
For example, people react very differently to carbohydrates like oats and sweet potatoes. Some people can eat oats with just a slight increase in blood sugar, while others see spikes quickly.
Simply knowing this allows those who are struggling with certain types of carbohydrates to choose to reduce their consumption or reduce their diet completely.
Protein and Fat
Carbohydrates have the most impact on blood sugar, but protein and fat also impact. Some people, like Dr. Sheri Colberg, one of the world’s leading voices on diabetes and exercise, believes looking at carbohydrates when estimating blood glucose shock (and administered insulin) is an outdated and inefficient way to pursue diabetes management.
In some expert opinions, you need to focus more on total calories (see here for more information on calorie counts and diabetes).
The important thing to note is that when protein and especially fat are consumed by carbohydrates, energy from the diet is released more slowly. This means that blood sugar levels will also be affected more slowly.
I don’t think your diabetes management should be entirely deciding how you live your life and which meals to follow, but it may be worth assessing which food choices make life easier for you.
By consciously choosing any type of nutrition plan (most of the time), you can more easily establish healthy habits that will benefit your overall health, as well as your daily blood sugar levels, and thus your A1C.
Increase your activities (exercise)
Exercise is essential to building and maintaining health, improving insulin sensitivity, but if you are constantly throwing blood sugar levels due to loops, it can become a double-edged sword. It can be very frustrating, scary, annoying, and annoying, as well as A1C and distance.
The key is to understand how different types of exercise affect your blood sugar levels and learn how to balance insulin and food around your workouts when using insulin.
Aerobic exercise
Aerobic exercises such as active walking, jogging, swimming, cycling and dancing are all excellent types of exercise. 20-30 minutes per day can make a big difference when it comes to improving insulin resistance and managing blood glucose levels.
Exercise not only reduces blood sugar during exercise, but also improves insulin sensitivity for a few hours after workout, meaning there is less insulin.
When treating diabetes with insulin, insulin levels should be controlled to avoid exercising exercise-induced hypoglycemia. This depends on significantly reducing insulin or consuming carbohydrates before training.
For many people, you may not need to “carbohydrates” to perform steady-state aerobic exercise for up to 60 minutes, but you will need to consume additional carbohydrates as there are situations where you cannot reduce your insulin before exercise.
It is also important to remember that different responses differ based on a variety of factors, such as insulin sensitivity, timing of the final insulin dose, and fitness level.
Resistance Training
Adding resistance training to your daily routine, such as free weights, weight machines, resistance bands, and body weight exercises, can help increase insulin sensitivity and lower A1C.
While aerobic exercise lowers blood glucose levels during exercise and potentially decreases about 48 hours after exercise, resistance training can increase insulin sensitivity much longer.
This is because the muscles mostly act as a “glucose tank” and store more glucose in the muscles rather than sending it directly into the bloodstream. The more muscles you have, the more sensitive you are insulin.
Note that some people will see a temporary increase in blood sugar levels during intense resistance training rather than decrease.
The reason for the increased blood glucose level is that the improvement in insulin sensitivity through exercise is exceeded by an increase in the body’s glucose production from the adrenaline released by activity.
This adrenaline causes the liver to break down glycogen and produce glucose, which the body produces glucose faster than it can use.
For a detailed guide, please read: How resistance training affects blood glucose levels.
Resistance training is very effective at increasing insulin sensitivity, so short-term effects aside, it is a great way to consistently lower blood sugar and A1c.
When exercise regularly, it has the effect of exercising overlap from one workout to the next, essentially achieving a permanent increase in insulin sensitivity. (Work with your medical team to tailor your treatment plan to avoid low levels from improving insulin sensitivity.)
Maintain a healthy weight
If you are overweight, losing 5-10% of your weight can help with a variety of health markers, including A1C levels.
In one study, people with type 2 diabetes who lost this amount of weight reduced A1C by an average of 0.5%.
How quickly can I lower the A1c?
The A1C test shows glucose over the past two to three months, so consistent diet and exercise changes for at least several weeks are required to see results reflected in A1C levels.
The exact time frame will vary based on individual factors such as the intensity of the change and the body’s response.
(This is simply due to the long-term nature of the test. That improvement is reflected much faster in glucose.)
In this video we will show you how to lower your A1C in 30 days following five simple steps.
Why is A1c too fast to lower?
We recommend that you lower the A1C with a little care. There are serious health risks associated with A1C too fast, just as the crash diet is not healthy.
I asked Dr. Anne Peters, director of the USC Clinical Diabetes Program, and a professor at the USC School of Clinical Medicine for an explanation.
Can your A1c be too low?
As mentioned above, the answer to this question will depend almost entirely on how often you experience hypoglycemia. If you (almost) experience no hypoglycemia and A1C is on the target, this suggests that your diabetes management is effective.
However, this does not mean that very low A1c is always safe or desirable. Each person’s ideal A1C levels may vary, and factors such as the risk of hypoglycemia discomfort, diabetes, age, and the amount of time that should be considered should be taken into consideration.
If you often experience hypoglycemia, it will result in a “artificial” low A1C read, as your hypoglycemia event lowers the average blood glucose level.
In that case, it is much more important to focus on increasing range than lowering A1c even further. In fact, they can even benefit from a slightly higher A1c with low blood glucose variability.
It is also important to note that lowering the generally recommended A1C of 6.0-7.0 percent has not been proven to provide health benefits. Therefore, a very low A1C should not be a target in itself.
What is a good A1C target??
Now that you have an A1C number, let’s see what it actually conveys. The American Diabetes Association has established the following guidelines:
| A1C level | What that means |
| Less than 5.7% | Normal (minimum risk of type 2 diabetes) |
| 5.7% to 6.4% | “Prediabetes” means you are at risk of developing type 2 diabetes |
| Over 6.5% | Diagnostic diabetes |
This does not mean that if you live with diabetes, you need less than 5.7% A1c. This means that if you don’t live with diabetes, your A1C is expected to be below 5.7%.
There are various recommendations as to what A1C is appropriate for people living with diabetes.
I had the opportunity to ask Dr. Peters and the author of the owner and clinical director of MS, CDCES, and Integrated Diabetes Services. Think of it like a pancreastheir perspective is on good A1C targets:
Dr. Peters:
bend:
Read more about A1c: What is “regular” HBA1c? and What are the dangerous levels of A1c?
To them Diabetes Care Standards – 2024the American Diabetes Association recommends an A1C target of less than 7.0% for adults living with diabetes.
7.0% A1c is roughly converted to an average blood glucose level of 154 mg/dL (8.6 mmol/L), as seen from this conversion chart (EAG represents “estimated average glucose”).
| A1c | Eco (mg/dl) | Eco (mmol) |
| 5% | 97 | 5.4 |
| 6% | 126 | 7.0 |
| 7% | 154 | 8.6 |
| 8% | 183 | 10.2 |
| 9% | 212 | 11.8 |
| 10% | 240 | 13.3 |
| 11% | 269 | 14.9 |
| 12% | 298 | 16.5 |
| 13% | 326 | 18.1 |
| 14% | 355 | 19.7 |
For more information about converting A1c to average glucose levels, see below. How to convert A1c to blood sugar levels.
A1C vs. Time in Long
A1C has long been considered the best measure of diabetes management as it was the most accurate tool for observing long-term blood glucose levels. This changed with the introduction of continuous glucose monitoring (CGM).
Using CGM allows you to take very accurate photos of not only average blood sugar, but also blood sugar fluctuations.
This allows you to track another important component of diabetes management.
A range refers to the percentage of time that blood sugar is within a certain range. To see why time within range is important, take a look at the three lines in the graph below.
All three strains show an average blood glucose level of approximately 154 mg/dL (8.6 mmol/L, an estimated average of approximately 7.0%), but the variation is very different. I think we all prefer blood sugar to follow line 3 rather than line 1.
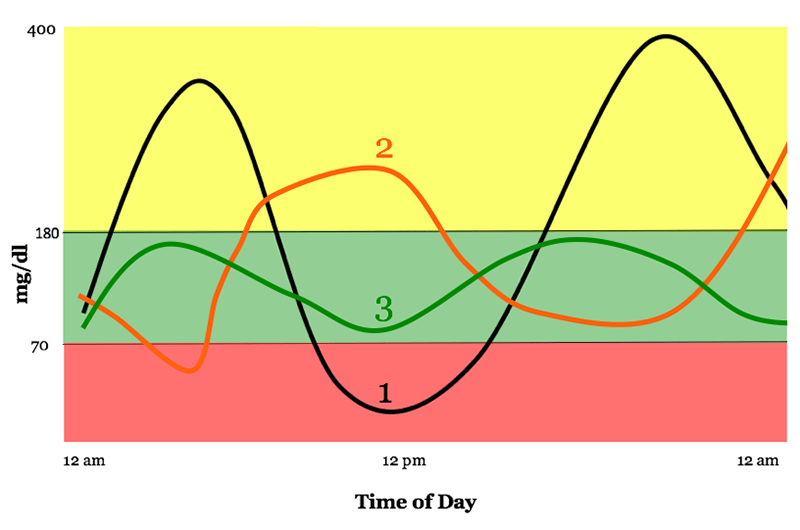
Graphs used with permission from diatribe.
Some guidelines state that blood glucose range should be set between 70 and 180 mg/dL (3.9 to 10 mmol/L), but you can see that it is too wide or too narrow.
In this interview with some diabetes experts, we recommend spending less than 3% of time under 70 mg/dL (3.9 mmol/L) and less than 1% of time under 54 mg/dL (3 mmol/L). But they also agree that the actual time spent on the range must be individualized.
On average, experts didn’t expect the general diabetes population to range from 50% or more at best, so talking about progressive improvements makes more sense than setting a fixed number.
Measurement method within the time
If you are wearing CGM, you must list the metrics within range when downloading data (as in the DEXCOM CGM example below).
Some CGM devices provide alerts when glucose levels are expected to fall into or leave the target range. This allows users to respond proactively and spend more time across the range.
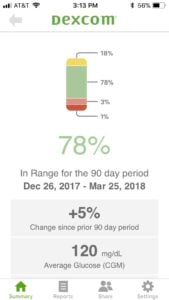
(Click to expand.)
Without CGM, all you can do is look at manual glucose readings and pay attention to high and hypoglycemic readings outside the target range.
Accepted highs and lows are things that need to be discussed with the medical team.
More importantly, is A1c low or high?
Ideally, A1c with hypoglycemic variability (high distance) could be less than 7.0%. Here are some good general guidelines:
- The higher the A1c, the more important it is to focus on defeating it.
- The lower the A1c, the more important range.
If A1C is below 6.0-7.0%, focusing on the increase within range will have a greater health impact than lowering A1C.
So, is A1C the best way to measure whether your diabetes management is going well? To quote Scheiner, although not necessarily:
Final Thoughts: My Perspective on A1c as a Person Living with Diabetes
I have a very vague relationship with myself. I have lived with type 1 diabetes for over 20 years, but my A1C is not something I think about in my daily life.
But every 3-6 months, looking at my end makes me feel a little uneasy as I get an A1C and get a diabetes report card.
And honestly, it’s really ridiculous. My A1C number does not reflect what’s been going on in my life for the past three months. I don’t know how much effort I put into managing my diabetes. And they don’t define me as a person. It’s a good source of information and nothing more.
Still, we tend to look at it, determine how we did it in diabetes management, and decide whether it’s good or bad. But we really shouldn’t!
That doesn’t mean you shouldn’t check A1C. I think we should definitely do it, but we also need to understand what that means and why we should look beyond the A1C number. We hope this guide will give you the knowledge and tools to do so.