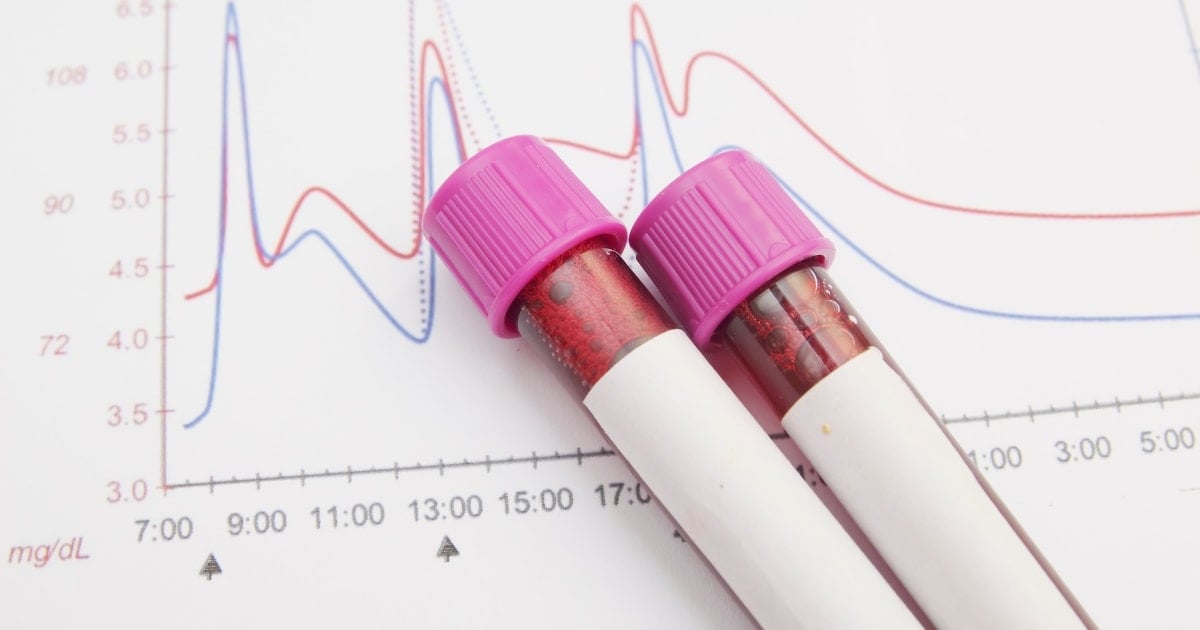
Understanding what your blood sugar levels are and what is considered “normal” can be confusing, especially if you have diabetes.
Blood glucose targets, or targets, can vary for everyone, and may vary from time to time to make it even more complicated.
This article will help you understand the target blood glucose and A1C levels in both people, with or without diabetes.
Blood glucose and A1C chart: normal and diabetic blood glucose range
learn more: What is normal blood sugar?
What is blood sugar?
Blood glucose, also known as blood glucose, is sugar found in the blood. This type of sugar is the main source of energy or fuel for the body. It is also the main source of energy in the brain.
When you eat, your body breaks down carbohydrates (carbohydrates) in your food into glucose, which is released into the bloodstream. As glucose levels in the blood begin to rise, the pancreas releases the hormone insulin and travels to cells that use glucose for energy.
How is blood sugar levels controlled in people who do not suffer from diabetes?
In people who do not suffer from diabetes, blood glucose levels are very closely controlled in the body by two hormones: insulin and glucagon. Excess glucose in the blood is stored as liver glycogen.
If your body needs extra glucose for fuel, for example, if you need fuel overnight while exercising or sleeping, glucagon will inform your liver and release glucose into the bloodstream. From there, insulin helps move that glucose into cells and use it for energy.
Why are diabetes and blood sugar levels important?
With diabetes, blood sugar levels may be too high. In the case of type 1 diabetes, the pancreas either produces or produces very little insulin. As a result, glucose from the blood cannot enter the cells for use in energy. In type 2 diabetes, cells in the body do not respond very well to insulin. Additionally, the pancreas stops producing enough insulin to regulate blood glucose.
Hyperglycemia is called hyperglycemia. If left untreated over time, this condition can lead to serious complications. These include:
Other problems caused by hyperglycemia include foot problems, periodontal disease, skin problems, and hearing loss.
Short-term, untreated hyperglycemia can cause potentially life-threatening complications such as:
In either case, immediate treatment is required.
Fasting blood sugar
Fasting blood glucose is the level of blood glucose measured or checked after fasting. “Fasting” means not eating or drinking anything except water for at least eight hours.
If you have diabetes and check your blood glucose level with a blood glucose meter, your health care provider may ask you to check your fasting blood glucose level. Depending on your sleep schedule, this is the first blood sugar check you do after you wake up, before eating breakfast or drinking morning coffee.
For most people with diabetes, the goal is fasting blood glucose between 80 and 130 mg/dL. Fasting blood glucose levels in people who do not suffer from diabetes should be between 70 and 99 mg/dL.
Fasting blood glucose above 130 mg/dL means that certain hormones have too high blood glucose (called the dawn phenomenon). Other possible causes of high fasting blood glucose include not having insulin or rebound hyperglycemia after undergoing hypoglycemia in the middle of the night.
Fasting blood glucose below 80 mg/dL means you are taking too many diabetic medications (including insulin). Another cause may be inadequate, being more active than usual, or drinking alcohol without eating.
Blood sugar after meal
Food has a big impact on blood sugar levels, so if you have diabetes, it can be helpful to check your blood sugar levels after meals. This is called post-meal or post-meal blood glucose checking and is intended to capture the “peak” or highest blood glucose level after eating.
The American Diabetes Association (ADA) proposes a target below 180 mg/dL for most non-pregnant adults 1-2 hours after the start of a meal. For people without diabetes, blood glucose levels usually remain below 140 mg/dL.
Blood glucose levels above 180 mg/dL after eating often mean that your diet may be too high in carbohydrates. For example, a pasta and Italian bread dinner is more likely to cause post-meal glucose “spikes” compared to a meal of grilled fish, vegetables and brown rice. However, high blood sugar levels after lactose can also occur because:
- Forget to take your diabetes medication
- Not taking sufficient diabetes medication
- Feeling unwell or stressful
- Not doing normal levels of physical activity
If the cause can be determined, occasional hyperglycemia after meals is normal. However, repeated post-pregnancy glucose levels can cause concern and may indicate the need to reduce carbohydrates or start or adjust diabetes medication.
High blood sugar levels
In people with diabetes, hyperglycemia is usually considered to be blood glucose above 180 mg/dL 1-2 hours after eating.
If your blood glucose level exceeds 180 mg/dL, symptoms of hyperglycemia can occur. These include feeling thirsty, needing frequent urination, fatigue, irritability, and blurry vision. Many people with diabetes start to experience symptoms of hyperglycemia when their blood sugar levels reach 250 mg/dL, which can vary from person to person.
Blood glucose levels reaching 400 mg/dL or higher may indicate the risk of the two serious conditions mentioned above.
DKA is more common in people with type 1 diabetes, but can also affect people with type 2 diabetes. High blood sugar and elevated ketones (chemicals produced by the liver when fat breaks down), rapid breathing, fruity-scented breathing, nausea, vomiting, and stomach pain can appear.
DKA could soon become a medical emergency. Treatment includes intravenous administration of insulin, as well as hospitalization replacing fluids and electrolytes.
HHS is a complication of type 2 diabetes, indicating very high blood sugar levels, extreme dehydration, reduced arousal, or even loss of consciousness. Treatment focuses on hospitalization, correct dehydration, replace electrolytes, and insulin intravenously administered.
See more details: What is considered hyperglycemia?
Hypoglycemia levels
Blood glucose levels fluctuate throughout the day in both people, with or without diabetes. For people with diabetes, the general goal is to aim to keep blood sugar levels between 80 mg/dL and 180 mg/dL (or the range recommended by the medical team).
Sometimes blood sugar levels get too low, below 70 mg/dl. This is called hypoglycemia. You may have symptoms that warn you of hypoglycemia, such as feeling unstable or a light head.
Not everyone has symptoms when they are low, so checking blood glucose levels frequently in meters, or, if possible, using CGM (continuous glucose monitoring) can help you identify when glucose levels are too low and too low. If this occurs, low carbohydrate sources should be treated to raise blood sugar levels to a safe level.
A too low blood sugar level (usually below 54 mg/dl) is called severe hypoglycemia, meaning that you need help from someone who can help treat and recover from the low ones. Severe hypoglycemia can lead to a risk of fainting. If blood sugar levels are too long or low, it can lead to seizures, coma, and rarely death. Treatment may include administration of glucagon by injection or inhalation, or intravenous glucose.
read more: What is considered hypoglycemia?
Individual blood glucose targets
The glucose goals listed in the table above are not necessarily appropriate for all people with diabetes. In fact, the ADA strongly recommends adjusting glucose targets as needed based on specific factors. These include:
- year: Elderly people with functional or cognitive disabilities, or very young children, may need higher glucose goals for safety and simplicity. However, young adults with no complications of diabetes may benefit from lower glucose goals.
- Health status: People with limited average life expectancy or limited certain medical conditions often have higher glucose targets.
- Risk of hypoglycemia: People who are not aware of hypoglycemia (cannot detect early signs of hypoglycemia) or who have severe hypoglycemia may have high blood glucose levels.
- Pregnant women with diabetes: Glucose goals are generally much tougher before and during pregnancy, and help to minimize mother and baby complications.
Talk to your healthcare provider about your glucose goals and what makes sense to you.
A1C Goals
The A1C test is a blood test that measures the average amount of glucose in your blood for the past 2-3 months. The results of this test are measured as percentages. Other terms for A1C are hemoglobin A1C, HBA1C, glycate hemoglobin, and glycosylated hemoglobin.
The A1C test is often used to diagnose pre-diabetes or diabetes, but it is also an important test that will help you and your medical team manage your diabetes. The higher the A1C level, the higher the risk of developing complications.
According to the ADA, the common target for A1C in most people with diabetes is less than 7%. For people without diabetes, the target is below 5.7%. A1Cs of 5.7% to 6.4% indicate prediabetics. This is a condition in which blood sugar levels are higher than normal, but not so high that it is considered type 2 diabetes.
Prediabetes means that you are at a high risk of developing type 2 diabetes. Fortunately, lifestyle changes can prevent or delay type 2 diabetes and other serious problems.
People with diabetes usually check A1C 2-4 times a year. If treatment goals are met, A1C checks are sufficient twice a year. However, if treatment goals are not met or treatment plans have changed, A1C checks may be frequently required.
Individual A1C goals
A1c below 7% may not be appropriate for everyone. The ADA states that “lower A1C goals are suitable for individuals with limited life expectancy and/or with significant functional and cognitive impairments.” For example, an A1C goal of up to 8% may be recommended for older people or those experiencing severe or frequent hypoglycemia.
For example, a low A1C goal of 6.5% may be suitable for young people with less frequent blood sugar levels. For pregnant women with diabetes, if this can be achieved without frequent hypoglycemia, the “ideal” A1C goal is less than 6%. Together you and your healthcare provider must determine the best A1C goal for you.
Final thoughts
If you have diabetes, it is important to know your blood sugar levels and A1C targets. Your blood sugar levels and A1C test results will help you know if you and your healthcare team are meeting your goals.
Although occasional use of A1c outside of blood glucose levels and target ranges is completely normal, consistently high or low blood glucose levels, or consistently high A1C results are indications that a course revision of the diabetes treatment plan is being shown.
Have an open dialogue with your doctor or other members of your medical team. Ask about glucose and A1C goals and discuss factors that can help you reach your target, such as medication, diet, and physical activity.