The frozen shoulders you may hear, but never think – never think until it happens. Unfortunately, by some estimates, compared to 2-10% of the general population, this is not uncommon for people with diabetes.
In this post, we will explain how to diagnose, prevent and treat frozen shoulders and how to avoid them if you have them.
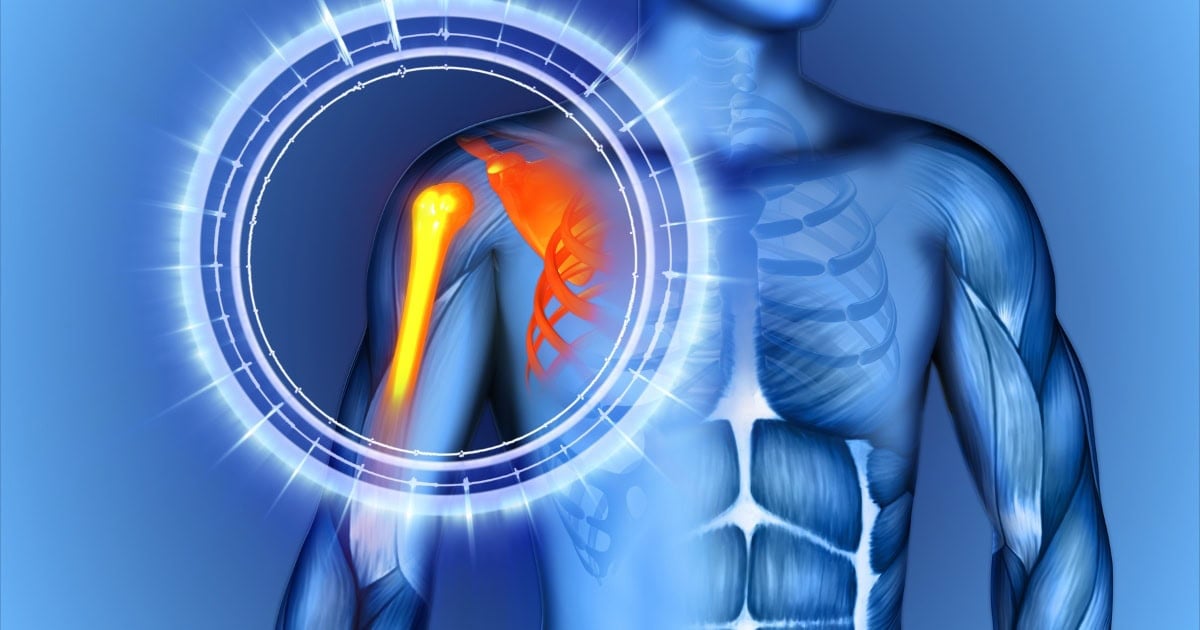
What is a frozen shoulder?
The frozen shoulder, also known as “adhesive caucitis,” gradually develops as the shoulder joints become stiffer, eventually becoming “freezing.”
This makes it difficult to lift your arms above your head or shoulder height, and any movement can cause serious pain. Over time, basic tasks like dressing and showering can become more challenging.
The exact link between diabetes and frozen shoulder is not fully understood, but it has been suggested that hyperglycemia forms the age (highly glycated end product) that stiffens tendons and ligaments.
This, combined with circulatory disorders, leads to inflammation and immobilization. People aged 40-60, especially women, are at higher risk, especially if they have had diabetes for many years.
How to diagnose frozen shoulders
This condition is usually diagnosed based on signs and symptoms.
The doctor will test both active range of motion (where you move your shoulder) and passive range of motion (where you move your shoulder). In both cases, limited movements often confirm the diagnosis.
How to prevent frozen shoulder intake
Unfortunately, there is no guaranteed method to prevent adhesive capitis.
However, reducing blood sugar levels can help reduce age formation, leading to joint stiffness and inflammation. Less age means lower risk of developing frozen shoulders.
read more: How to Lower A1C: A Complete Guide.
Beyond that, maintaining a consistent stretch and physical activity routine is important to maintaining range of motion in the shoulder. You don’t have complete control over whether or not you freeze your shoulders, but you can get the best possible results.
Timeline for developing states
Early signs are very subtle and you may not notice them, so it is important to keep in mind persistent shoulder pain and stiffness.
Most frozen shoulders ultimately improve on their own, but the process is slow and involves various stages of discomfort. Freeze, freeze, thaw.
The freezing stage lasts for about 6 weeks to 9 months, with the most intense pain and limited movement. During the frozen stage, pain decreases, but mobility remains severely restricted, usually lasting for 4-6 months.
Treatment Options
Most people choose non-surgical treatments first, such as physical therapy or non-steroidal anti-inflammatory drugs (NSAIDs) like ibuprofen.
Others consider steroid injections to reduce joint pain and improve range of motion.
However, if you have diabetes, it is important to know that steroid injections can cause a significant increase in blood glucose levels up to a week. Always consult with your care team before pursuing this type of treatment.
These non-surgical measures are effective for many people. However, if symptoms do not improve, more intensive options such as the release of an open cap coronary or arthroscopic surgery may be recommended for physiotherapy.
Exercise and stretches that help treat frozen shoulders
Jenna Peitz, physiotherapist at Accelerated PT & Wellness, offers the following advice:
Below are two exercises she recommends to help you regain your shoulder range of motion.
Table slides/table walk
Sit at the table with your palms down. Lift forward with your hips and slide your hands out of your body. If it hurts too much, point your thumb before starting.
Mackenzie’s method of repeating shoulders
Stand at the table or counter and place your hands. As you turn from your arms, rotate your palm towards your thumb. Crouch down until it feels tight, then relax and repeat.
These low-intensity exercises can be performed four to six times a day with a set of 10 to 20 reps.
Unlike typical exercises, the focus here is on regaining range of motion. So volume and strength are not that important.
All cases are different, so it’s important to consult a physical therapist about exercise tailored to your situation, says Pats, but these are good starting points.
If you have frozen shoulders, what should you do
There are a few things that may seem helpful, but can actually make this condition worse.
Do not use shoulder slings
While keeping your shoulders in place to relieve pain is attractive, limiting movement can lead to worsening stiffness. Use your arms to maintain that range of motion (unless your doctor specifically recommends a sling after surgery).
Don’t stop using your arms completely
Despite the pain, the arms are gently moved to help with the healing process. Avoid lifting heavy objects.
Don’t look for “magic treatment”
Frozen shoulders take longer to improve, and many websites will encourage simple fixes, but most of these remedies are ineffective and potentially harmful.
Take control: DO and DOS for frozen shoulders
While frozen shoulders affect many people living with diabetes, there is much to do to prevent or treat frozen shoulders.
- Keep your blood sugar levels as much as possible.
- Before developing frozen shoulders, exercise and stretch them regularly.
- Treat pain with anti-inflammatory drugs (NSAIDs).
- Work with a physical therapist to strengthen your shoulders and increase your range of motion.
- If nothing else goes well, you can consider surgery.
- Do not use shoulder slings or stop using your arms completely.
A frozen shoulder can be painful and can limit you with much of your daily activity, but the good news is that if you handle it correctly, the condition will almost always disappear in the end.
You got this!
Was this article helpful? (Yes) or click “No” to let us know!