Suffering from both hyperglycemia and hypoglycemia is almost an expected part of life with diabetes.
However, reactive hypoglycemia differs from normal hypoglycemia levels as people with diabetes encounter different underlying causes.
In this article, we’ll explain everything you need to know about reactive hypoglycemia: what it is, how to manage it, and how to better prevent it.
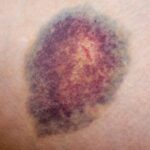
Symptoms of hypoglycemia
It is important to recognize symptoms of hypoglycemia before hypoglycemia becomes an emergency.
Hypoglycemia is usually defined as blood glucose levels below 70 mg/dL. Even people without diabetes can experience hypoglycemia!
Here are some notable signs:
- Shakin
- Dizziness
- anxiety
- It’s difficult to concentrate
- sweating
- confusion
- Rapid Heartbeat
- Feeling weakness and extreme fatigue
- It feels faint
- Hungry
- In severe cases, loss of consciousness, coma, and death
If you suffer from frequent hypoglycemia and do not suffer from diabetes, you should consult your doctor.
What is reactive hypoglycemia?
Reactive hypoglycemia (also known as post-meal hypoglycemia) is a type of hypoglycemia that occurs after meals, usually 2-5 hours after finishing your meal.
This is different from the hypoglycemia of fasting. The cause is that too much insulin is released in the food eaten.
There are three different types of reactive hypoglycemia.
Digestively reactive hypoglycemia – This is the form of reactive hypoglycemia that occurs approximately two hours after the meal is finished.
Idiopathic reactive hypoglycemia – This is the form of reactive hypoglycemia that occurs approximately 3 hours after the meal is finished.
Late reactive hypoglycemia – This form of reactive hypoglycemia occurs 4-5 hours after the meal is finished.
What causes reactive hypoglycemia?
The researchers are unclear about the exact cause of reactive hypoglycemia. However, people who often suffer from reactive hypoglycemia usually suffer from diabetes or diabetes and suffer from gastrointestinal dysfunction, such as gastroparesis.
Additionally, people who do not suffer from diabetes but have hormone deficiency may also suffer from reactive hypoglycemia.
Reactive hypoglycemia can be caused by gastric bypass or ulcer surgery, especially when recovering from cancerous tumors, excessive alcohol consumption, or surgery.
Reactive hypoglycemia usually occurs more frequently in overweight and obese people. In fact, suffering from reactive hypoglycemia, particularly late-stage reactive hypoglycemia, can increase your risk of developing diabetes.
How can I manage reactive hypoglycemia?
If you have reactive hypoglycemia and do not think you have diabetes, ask your doctor about getting a mixed resistance test (MMTT).
Here, they give you a sweet drink made to raise blood sugar levels, allowing your body to produce more insulin. Your doctor will closely track your blood sugar levels over the next few hours to see if there are spikes and then crashes.
It may drop too much after a few hours after taking the liquid (below 70 mg/dL), which can be a sign of suffering from reactive hypoglycemia.
If you currently have insulin-dependent diabetes, talk to your doctor about lowering the insulin-to-carbohydrate ratio, taking long-acting insulin, or both.
If you suffer from hypoglycemia after meals, you have diabetes, but if you are not using insulin, talk to your doctor about the potential lowering of diabetes medication.
However, if you’ve tried all of that and still have a failed treatment, below are some strategies for implementation to help you manage reactive hypoglycemia.
It is important to note that there is no clinical “treatment” for reactive hypoglycemia, but only methods that diminish the pancreas’ response to foods that help prevent such hypoglycemia after meals.
First, treat hypoglycemia
Repairing reactive hypoglycemia in general is different from treating acute episodes of hypoglycemia.
Eat at least 15 grams of fast-acting carbohydrates, such as glucose tablets, juices, or other sweets like candies, and test your blood sugar levels again to make sure it’s rising.
If you’re dangerously low and your blood sugar levels are not responding to fast-acting glucose, call 911 immediately and have someone give you glucagon.
Eat smaller, more consistent foods
Try to eat meals and snacks every 2-3 hours. Then don’t starve. When you eat, make sure it’s a huge meal and not a huge carb dump. This helps prevent the pancreas from being too much insulin, resulting in lower blood sugar levels.
You don’t eat all day, and eating a breathtakingly large amount of food increases reactive hypoglycemia attacks and plummets your blood sugar levels while you’re ready for sleep.
Focus on fats and proteins
When eating or eating snacks, make sure it’s packed with protein and healthy fats, not simple carbohydrates.
Diets and snacks with many processed added sugars and carbohydrates require more insulin, which is more likely to lead to reactive hypoglycemic episodes.
Healthy proteins and fats include foods such as salmon, full-fat dairy products such as Greek yogurt, peanut butter, and seeds and nuts, as well as extra virgin olive oil, coconut, avocados and lean meat.
You can easily make meals around these groceries by adding lush greenery and colorful vegetables that do not cause blood sugar and insulin spikes.
If you drink alcohol, don’t do that on an empty stomach
If you are susceptible to hypoglycemic levels and reactive hypoglycemia and enjoy drinking alcohol, always drink it with food.
Alcohol can lower blood sugar levels and put diabetics (even without!) at risk of hypoglycemia if you don’t have anything to eat for several hours.
Better yet, alcohol and high-fat, high-protein snacks will help ensure smoother blood sugar levels throughout the night. Think cheese, olives and raw vegetables with hummus and with wine.
Exercise regularly
It is important to do regular exercise that will help you maintain consistent blood sugar levels throughout the day. You aim to exercise early in the morning or afternoon, where you are most likely to be insulin resistant (and you are the least likely to be lower).
If you are struggling with reactive hypoglycemia after dinner, it is not the best time to exercise. However, establishing an exercise routine at the same time every day can help you learn how to respond to both carbohydrates and physical activity, reducing the chances of severe hypoglycemic levels.
If you’re not sure where to start, talk to your doctor about developing an exercise routine that works for you and your lifestyle.
Conclusion
Reactive hypoglycemia is a type of hypoglycemia that occurs after meals.
People with or without diabetes can suffer from this condition, but those who are overweight or obese, have prediabetics, have gastrointestinal problems such as diabetes or gastroparesis, and who are recovering from surgery are suffering from alcoholism or have cancerous tumors or hormonal imbalances.
There are several ways to manage reactive hypoglycemia. If you have first diabetes, lower your diabetes medication or insulin. Talk to your doctor about how to do this safely.
Treat hypoglycemia levels below 70 mg/dL immediately and call 911 if you are experiencing severe hypoglycemia that is not responding to treatment.
In the long term, you can choose to eat a smaller, more consistent diet focused on healthy fats and proteins, exercise regularly in the mornings, and drink alcohol alone along with food.
By taking these strategic measures, you can manage reactive hypoglycemia and prevent it from taking over your day.